Why are single embryo transfers usually recommended?
Prior to the fresh or frozen embryo transfer process, physicians and patients must decide how many embryos (and which specific embryo(s)) to transfer. Women are usually advised to transfer one single embryo to minimize risks to herself and the baby.
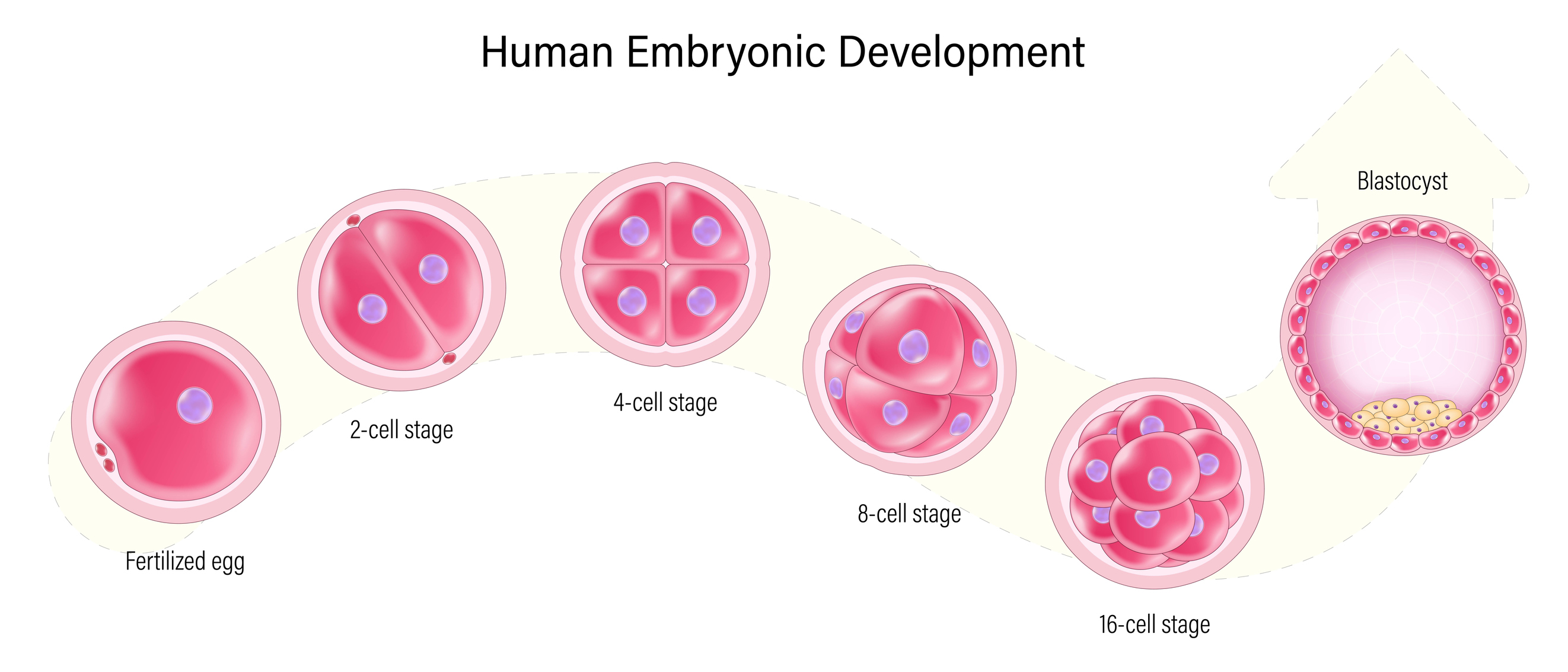
Embryo transfer is the last step of in-vitro fertilization (IVF), during which an embryo is placed into the uterus to achieve a pregnancy.i Fresh embryo transfer is usually performed on either day 3 or day 5 following egg retrieval and fertilization (day 0),ii though embryos can also be cryopreserved (frozen) and transferred in a subsequent cycle(s). Using previously cryopreserved embryos is called a frozen embryo transfer (FET).
SETs are preferred because they are far more likely than multiple embryo transfer to lead to singleton gestation (a single pregnancy), rather than a multiple gestation pregnancy (i.e., twins, triplets, etc.).iii A 2022 systematic review demonstrated a 16.7 percent chance of multiple gestation pregnancy after IVF when two embryos were transferred, compared to a 0.7-1.0 percent chance of multiple gestation after IVF with an SET.iv This data has been supported by other studies as well.v Singleton pregnancies offer decreased risk to both mother and baby, as discussed below. In addition, the costs to the health care system are significantly increased for twin or triplet pregnancies, including during delivery and postnatal care (especially due to increases in neonatal intensive care).vi,vii,viii
Risks of twin and multiple pregnancies
Single gestation pregnancies are preferred because they carry a significantly lower risk of maternal and fetal complications than multiple gestation pregnancies.ix,x A summary of the complications occurring most commonly in multiple gestation pregnancies is outlined below.
Maternal complications:
Postpartum hemorrhage: Multiple gestation pregnancies are more likely to result in severe bleeding after delivery, a condition known as postpartum hemorrhage. This is due to more extreme distention/stretching of the uterus required to accommodate multiple fetuses, which can lead to impaired uterine contractions, required to stop bleeding after delivery.xi
Hypertensive disorders of pregnancy: The incidence of gestational hypertension (high blood pressure), preeclampsia, and eclampsia are increased in multiple gestation pregnancies. In one 2021 study, the incidence of hypertensive disorders in singleton pregnancies was 6.5 percent, compared to 12.7 percent in twin and 20.0 percent in triplet pregnancies.xii Complications resulting from these disorders, such as kidney failure, heart attack, preterm delivery, restricted fetal growth and stroke, are also increased in multiple gestation pregnancies.xiii
Heterotopic pregnancy: This occurs when one pregnancy is intrauterine (within the uterus), while another is ectopic (implants somewhere other than the uterus, i.e., in the fallopian tube). While the intrauterine pregnancy is viable, the ectopic pregnancy is not, and may cause life-threatening bleeding for the mother if the pregnancy ruptures.xiv,xv
Neonatal complications:
Preterm delivery: There is an increased risk of preterm delivery in multiple gestation pregnancies. One study demonstrated that in twin pregnancies, the rate of preterm birth at < 37 weeks was 5.7 times higher than in a singleton pregnancy; delivery at < 32 weeks was 7.1 times more likely in twin compared to single pregnancies.xvi The resultant prematurity of a preterm delivery can cause significant neonatal morbidity such as breathing and feeding issues, as well as lasting neurologic problems and even neonatal death.xvii
Twin-twin transfusion syndrome (TTTS): This is a complication that can occur in certain types of twin pregnancies, where the twins share a placenta (monochorionic) but have two separate amniotic sacs (diamniotic). In TTTS, the blood flow from the placenta is not shared equally between the two fetuses, meaning one fetus gets more blood flow from the placenta and one has less. This results in one twin being growth-restricted and anemic, with less amniotic fluid (oligohydramnios). The other twin often has too high of a blood volume (hypervolemia), putting them at risk for heart failure, and has excess amniotic fluid surrounding them (polyhydramnios). These abnormalities can cause severe complications for both fetuses and lead to a high rate of fetal demise.xviii
Other risks include an increased risk of miscarriage, Caesarean section, premature preterm rupture of membranes, low birth weight, and perinatal (newborn) death.xix
When should a patient transfer only one embryo?
SETs are almost always recommended, but there are certain situations where fertility clinics are even more unlikely to allow the transfer of two embryos. The American Society of Reproductive Medicine (ASRM) has clear committee guidelines outlining standard practices for embryo transfer.
Age
One important factor is age. When transferring an embryo that has not been genetically tested, if an individual is less than 35 years of age, ASRM guidelines strongly encourage that only one embryo be transferred. For those aged 35-37 years, the recommendation is that there should still be a strong consideration for selecting SET only. For those above the age of 37 who are using their own eggs, more consideration may be made to transferring more than one embryo, which is discussed below in the section on multiple embryo transfer.xx This age-based stratification is supported by a study by Wang et al (2022) which arranged patients by age and investigated the first cycle of cleavage-stage (day 3) frozen embryo transfer where two embryos were transferred. They found that in patients less than 35 years old, the live birth rate per cycle was 59.6 percent and the rate of multi-pregnancy was 35.2 percent. For patients 36-37 years, the live birth rate was 48.2 percent, and the rate of multi-pregnancy was 27.1 percent. For patients over 38 years, the live birth rate was 33.3 percent, and the rate of multi-pregnancy was 18.9 percent.xxi While this study did not assess blastocyst (day 5 embryo) transfer, the results demonstrate that patient age is often the predominant consideration when deciding to transfer only a single embryo.xxii
Embryo Genetics
Embryo quality, based on genetic testing, is another important consideration when deciding how many embryos to transfer. Preimplantation genetic testing for aneuploidy (PGT-A) can be used to determine whether an embryo has the correct complement of chromosomes (euploid) or not (aneuploid). One randomized study of 205 couples demonstrated that transfer of a single euploid embryo had the same pregnancy rate as transfer of two untested embryos, but with a significantly lower rate of twin pregnancy.xxiii Thus, euploid embryos are considered favorable for transfer, and ASRM guidelines recommend that only one euploid blastocyst is transferred, regardless of age.xxiv
Embryo Grading
IVF clinics also use embryo grading – or methods of rating the quality of the embryo on factors such as their rate of replication and appearance under a microscope - to further quantify risk of multiple gestation with higher order embryo transfer. Another scenario where SET is strongly advised is when there is more than one high-quality embryo available for transfer. This recommendation is based on evidence that transferring two high-quality blastocysts leads to multiple gestation pregnancies in up to 50-60 percent of cases.xxv
Cycle Number
The number of prior embryo transfers an individual has attempted and how many have led to successful pregnancies is also an important factor. The ASRM practice committee strongly recommends SETs for the first or second IVF cycle, especially if an individual has had a previous successful IVF cycle.xxvi
Gestational Carrier
When the embryo is going to be transferred to a gestational carrier (surrogate), a single-embryo transfer is strongly recommended to minimize the risks of multiple gestation pregnancies to the gestational carrier.xxvii,xxviii
Other Reasons
There are many personal reasons that individuals may decide to transfer only a single embryo. Some of these reasons include previous pregnancy complications, a strong desire to avoid a twin pregnancy or twin parenting, and concern about increased healthcare expenses associated with multiple gestation pregnancies.xxix
When is single embryo transfer mandatory?
While a SET is typically recommended, there are certain circumstances where it may be mandatory. For example, clinics may have a policy for mandatory SET (for certain age groups) to minimize maternal and neonatal risks of multiple gestation pregnancy. In addition, SET is often considered mandatory for patients with certain anatomic anomalies including a unicornuate uterus or uterine didelphis, and those with significant health problems such as heart disease, lupus, kidney issues or high blood pressure. This is because the risk of complications from a multiple gestation pregnancy is unacceptably high in these patients.
Also, in some regions or countries where universal healthcare or private insurance covers IVF costs, there are regulations where only SETs are permitted, with some exceptions for advanced maternal age. These policies are in place to avoid the increased health care costs incurred by twins and higher order multiples.xxx Similarly, in countries with privatized insurance, such as the United States, some healthcare insurance policies mandate a SET in order to similarly lessen the chance of higher costs. Interestingly, studies demonstrate that patients in states where insurers are required to cover IVF are more likely to use SET compared to those paying out-of-pocket for IVF, likely because the additional FET costs are less of a factor for those with adequate insurance coverage.xxxi,xxxii,xxxiii In one study, live birth rate was found to be higher and multiple birth rates found to be lower in states with IVF insurance coverage compared to those without mandated coverage.xxxiv
Why do patients transfer two or more embryos?
There are various cases where patients and their providers decide that the potential benefits of transferring >2 embryos outweigh the risks.
Patients are most likely to consider a double or multiple embryo transfer to increase the chance of success. When transferring two or more genetically untested embryos, there is a higher likelihood of pregnancy and live birth for that cycle, compared to SET.xxxv However, it is important to note that the increased success rates are per transfer and may not reflect an improved cumulative live birth rate. This means that while multiple embryo transfer has higher odds of success on that specific transfer, this does not necessarily mean that the there is a higher odd of pregnancy when considering all transfers resulting from the same egg retrieval. In other words, each embryo has its own capacity to lead to pregnancy so if the second embryo is transferred later, the overall pregnancy is expected to be the same. The research comparing success rates in single versus double (or more) embryo transfers is discussed later in this article.
As discussed below, patients consider transferring multiple embryos for various medical, financial, and personal reasons.
Medical reasons for transferring two or more embryos
The risk for a twins or triplets pregnancy is often lower for untested embryos at older ages, with transfer of low-quality embryos, and in the setting of repeated implantation failure (RIF). In these situations, the patient may choose to transfer more than one embryo to increase the odds of successful transfer.
For women using their own eggs, resultant embryos are more likely to be aneuploid and fail implantation as they get older, especially after the age of 40.xxxvi As such, there is lower risk for multiples occurring with embryo transfer with advanced age if the embryos are not genetically tested,xxxvii meaning that physicians and patients are more likely to be comfortable transferring two or more embryos.
According to ASRM guidelines, for patients with untested embryos (no preimplantation genetic testing) and other unfavorable conditions, the following number of cleavage stage (Day 2-3) embryos or blastocysts (Day 5-6) can be considered for transfer:xxxviii
35-37yr: up to 3 cleavage stage embryos; up to 2 blastocysts
38-40yr: up to 4 cleavage stage embryos; up to 3 blastocysts
41-42yr: up to 5 cleavage stage embryos; up to 3 blastocysts
Unfavorable conditions include cases where there are no high-quality embryos available, lack of embryos for cryopreservation, or previous failed transfers.
Another scenario where it may be appropriate to transfer an extra embryo is in patients that have a favorable prognosis, but have had multiple unsuccessful cycles, such as repeated implantation failure.xxxix
Financial, logistical, and other considerations for transferring 2+ embryos
Aside from medical reasons for transferring more than two embryos, there are also various financial and logistical reasons that an individual may consider. The costs associated with future embryo transfers - the procedure, transfer medications, embryo cryopreservation fees, time away from work, travel costs - often deter patients from choosing elective SET. A double or triple embryo transfer allows patients to avoid these costs again, which can be a significant incentive for those paying out-of-pocket for IVF.
Although patients themselves may incur higher costs, SET is more cost-effective for the healthcare system, since the cost of multiple gestation pregnancy is very high.xl,xli,xlii,xliii One 2020 health economics study investigating cost-effectiveness in a US state with no fertility coverage showed that SET can result in significant savings for the medical system. The study found that SET saves ~$3.5 million USD per 250 patients; however, they found that costs to the patient were higher in SET ($23,036), compared to double embryo transfer (DET) ($20,535).xliv
Some patients may be concerned about cryopreservation of embryos, and therefore prefer transfer of multiple embryos at once to prevent the need to freeze embryos. However, the process of vitrification with rapid cooling has been shown to produce very high post-thaw survival rates (i.e., above 97 percent).xlv,xlvi Therefore, SET should still be considered in cases where this is the primary concern.
In some countries, there are additional considerations that may justify transferring more than one embryo. For example, in locations with limited embryo storage facilities, high costs for storage, or religious concerns about the fate of additional embryos, these factors may justify transferring multiple embryos.xlvii It is important to acknowledge that some insurance policies and fertility clinics may include stipulations about the number of embryos that can be transferred per cycle.
Success rates of embryo transfer with single vs multiple embryos
Multiple factors impact the success rates of a single embryo versus multiple embryos (during one embryo transfer cycle). When transferring two or more embryos, there is an increased chance of pregnancy and live birth for that cycle (per transfer rate), compared to SET.xlviii
A Cochrane review (2020)xlix found that a woman with a 46 percent chance of live birth following one IVF cycle with DET of untested embryos, had a 27-36 percent chance of live birth following one IVF cycle with SET. Therefore, there was a reduced rate of pregnancy following SET compared to DET for a single cycle of IVF (as expected). The risk of multiple gestation pregnancy was found to be higher in the DET group.
In one large study of over 180 000 good prognosis cases, DET increased the chance of success by 10-15 percent over SET, but significantly increased the risk of multiples; the rate of twin births was 2 percent in SET and 49 percent in DET.l
Similar higher live birthrates following DET have been shown in studies using cleavage stage embryos (Day 2 or Day 3 embryos). One study demonstrated that cleavage stage SET had a lower single cycle live birth rate (27 percent) compared to DET (42 percent), but also had a five times higher rate of singleton gestation vs multiple gestation.li,lii
However, transferring multiple embryos in a single cycle does not improve the cumulative success rate of an IVF cycle. In other words, considering the total odds of live birth using all embryos from a single IVF cycle, evidence shows that SET has similar success rates, while having the added benefit of lower risk for multiples.liii,liv,lv,lvi For example, the same Cochrane review described abovelvii also looked at cumulative live birth rates. The study found that the live birth rate after one cycle of DET (42 percent) was similar to the cumulative live birth rate of repeat cycles of SET (34-46 percent).lviii
A 2022 meta-analysis of 12 studies (almost 200 000 women) compared one DET vs. two cycles of SET.lix They found that the cumulative live birth rate was similar with two cycles of SET, compared to one cycle of DET. As expected, SET also resulted in a lower incidence of multiple gestation pregnancies, prematurity, and low birth rate.lx Another large retrospective cohort study even showed that choosing SET on the initial cycle was associated with higher cumulative live birth rates (74 percent) compared to those initially choosing DET (57 percent).lxi These studies demonstrate that each embryo has its own capacity to lead to pregnancy.
Conclusion
While a single embryo transfer is usually promoted, research across multiple peer reviewed journals has highlighted various factors where a woman and/or practitioner may feel that transferring more than one embryo is beneficial for that individual. Patients should speak to their healthcare provider to discuss which option is best, but being informed on the various considerations can help them feel at ease when making this decision.
i Barton, S. E., & Ginsburg, E. S. (2012). Oocyte retrieval and embryo transfer. In Vitro Fertilization, 55-74. https://doi.org/10.1007/978-1-4419-9848-4_4
ii Letterie, G., et al. (2005). The relationship of clinical response, oocyte number, and success in oocyte donor cycles. Journal of Assisted Reproduction and Genetics, 22(3), 115-117. https://doi.org/10.1007/s10815-005-4875-9
iii Criteria for number of embryos to transfer: A committee opinion. (2013). Fertility and Sterility, 99(1), 44-46. https://doi.org/10.1016/j.fertnstert.2012.09.038
iv Ma, S., et al. (2022). Comparisons of benefits and risks of single embryo transfer versus double embryo transfer: A systematic review and meta-analysis. Reproductive Biology and Endocrinology, 20(1). https://doi.org/10.1186/s12958-022-00899-1
v Ozturk, O., et al. (2001). Number of embryos for transfer following in-vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd003416
vi Ory, S., et al. (2020, July 20). Successful implementation of a mandatory single embryo transfer (SET) program: how we did it. Fertility & Sterility. https://www.fertstert.org/news-do/successful-implementation-mandatory-single-embryo-transfer-set-program-we-did
vii Lukassen, H., et al. (2004). Cost analysis of Singleton versus twin pregnancies after in vitro fertilization. Fertility and Sterility, 81(5), 1240-1246. https://doi.org/10.1016/j.fertnstert.2003.10.029
viii Van Heesch, M. M., et al. (2010). Long term costs and effects of reducing the number of twin pregnancies in IVF by single embryo transfer: The TwinSing study. BMC Pediatrics, 10(1). https://doi.org/10.1186/1471-2431-10-75
ix Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
x Raffé-Devine, J., et al. (2022). Maternal, fetal, and neonatal outcomes of elective fetal reduction among multiple gestation pregnancies: A systematic review. Journal of Obstetrics and Gynaecology Canada, 44(1), 60-70.e12. https://doi.org/10.1016/j.jogc.2021.07.020
xi Ende, H. B., et al. (2021). Risk factors for atonic postpartum hemorrhage. Obstetrics & Gynecology, 137(2), 305-323. https://doi.org/10.1097/aog.0000000000004228
xii Narang, K., & Szymanski, L. M. (2020). Multiple gestations and hypertensive disorders of pregnancy: What do we know? Current Hypertension Reports, 23(1). https://doi.org/10.1007/s11906-020-01107-4
xiii Narang, K., & Szymanski, L. M. (2020). Multiple gestations and hypertensive disorders of pregnancy: What do we know? Current Hypertension Reports, 23(1). https://doi.org/10.1007/s11906-020-01107-4
xv Mashamba, T. (2023). Complications of multiple pregnancy: Conception to delivery. Multiple Pregnancy - New Insights. https://doi.org/10.5772/intechopen.107293
xvi Li, S., et al. (2021). Perinatal outcomes and risk factors for preterm birth in twin pregnancies in a Chinese population: A multi-center retrospective study. Frontiers in Medicine, 8. https://doi.org/10.3389/fmed.2021.657862
xvii Li, S., et al. (2021). Perinatal outcomes and risk factors for preterm birth in twin pregnancies in a Chinese population: A multi-center retrospective study. Frontiers in Medicine, 8. https://doi.org/10.3389/fmed.2021.657862
xviii Dudenhausen, J. W., & Maier, R. F. (2010). Perinatal problems in multiple births. Deutsches Ärzteblatt international. https://doi.org/10.3238/arztebl.2010.0663
xix Mashamba, T. (2023). Complications of multiple pregnancy: Conception to delivery. Multiple Pregnancy - New Insights. https://doi.org/10.5772/intechopen.107293
xx Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
xxi Wang, Z., et al. (2022). Clinical outcomes after elective double-embryo transfer in frozen cycles for women of advanced maternal age. Medicine, 101(9), e28992. https://doi.org/10.1097/md.0000000000028992
xxii Ma, S., et al. (2022). Comparisons of benefits and risks of single embryo transfer versus double embryo transfer: A systematic review and meta-analysis. Reproductive Biology and Endocrinology, 20(1). https://doi.org/10.1186/s12958-022-00899-1
xxiii Forman, E. J., et al. (2013). In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertility and sterility, 100(1), 100–7.e1. https://doi.org/10.1016/j.fertnstert.2013.02.056
xxiv Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
xxv Elective single-embryo transfer. (2012). Fertility and Sterility, 97(4), 835-842. https://doi.org/10.1016/j.fertnstert.2011.11.050
xxvi Elective single-embryo transfer. (2012). Fertility and Sterility, 97(4), 835-842. https://doi.org/10.1016/j.fertnstert.2011.11.050
xxvii Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
xxviii Elective single-embryo transfer. (2012). Fertility and Sterility, 97(4), 835-842. https://doi.org/10.1016/j.fertnstert.2011.11.050
xxix Lee, A. M., et al. (2016). Elective single embryo transfer- the power of one. Contraception and Reproductive Medicine, 1(1). https://doi.org/10.1186/s40834-016-0023-4
xxx Ory, S., et al. (2020, July 20). Successful implementation of a mandatory single embryo transfer (SET) program: how we did it. Fertility & Sterility. https://www.fertstert.org/news-do/successful-implementation-mandatory-single-embryo-transfer-set-program-we-did
xxxi Peipert, B. J., et al. (2022). Impact of in vitro fertilization state mandates for third party insurance coverage in the United States: A review and critical assessment. Reproductive Biology and Endocrinology, 20(1). https://doi.org/10.1186/s12958-022-00984-5
xxxii Zagadailov, P., et al. (2020). Do state insurance mandates alter ICSI utilization? Reproductive Biology and Endocrinology, 18(1). https://doi.org/10.1186/s12958-020-00589-w
xxxiii Peipert, B. J., et al. (2022). Impact of comprehensive state insurance mandates on in vitro fertilization utilization, embryo transfer practices, and outcomes in the United States. American Journal of Obstetrics and Gynecology, 227(1), 64.e1-64.e8. https://doi.org/10.1016/j.ajog.2022.03.003
xxxiv Peipert, B. J., et al. (2022). Impact of comprehensive state insurance mandates on in vitro fertilization utilization, embryo transfer practices, and outcomes in the United States. American Journal of Obstetrics and Gynecology, 227(1), 64.e1-64.e8. https://doi.org/10.1016/j.ajog.2022.03.003
xxxv Richter, K. S., et al. (2016). Factors associated with birth outcomes from cryopreserved blastocysts: Experience from 4,597 autologous transfers of 7,597 cryopreserved blastocysts. Fertility and Sterility, 106(2), 354-362.e2. https://doi.org/10.1016/j.fertnstert.2016.04.022
xxxvi Morris, J., et al. (2021). The rate of aneuploidy and chance of having at least one euploid tested embryo per ivf cycle in 21,493 preimplantation genetic screening for aneuploidy (pgt-a) tested embryos as determined by a large genetic laboratory. Fertility and Sterility, 116(1), e15. https://doi.org/10.1016/j.fertnstert.2021.05.024
xxxvii Mejia, R. B., et al. (2021). Elective transfer of one embryo is associated with a higher cumulative live birth rate and improved perinatal outcomes compared to the transfer of two embryos with in vitro fertilization. F&S Reports, 2(1), 50-57. https://doi.org/10.1016/j.xfre.2020.10.011
xxxviii Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
xxxix Guidance on the limits to the number of embryos to transfer: A committee opinion. (2021). Fertility and Sterility, 116(3), 651-654. https://doi.org/10.1016/j.fertnstert.2021.06.050
xl Jaspal, R., et al. (2019). The impact of cross-border IVF on maternal and neonatal outcomes in multiple pregnancies: Experience from a UK fetal medicine service. European Journal of Obstetrics & Gynecology and Reproductive Biology, 238, 63-67. https://doi.org/10.1016/j.ejogrb.2019.04.030
xli Bahadur, G., et al. (2020). Observational retrospective study of UK national success, risks and costs for 319,105 IVF/ICSI and 30,669 IUI treatment cycles. BMJ Open, 10(3), e034566. https://doi.org/10.1136/bmjopen-2019-034566
xlii Lukassen, H., et al. (2004). Cost analysis of Singleton versus twin pregnancies after in vitro fertilization. Fertility and Sterility, 81(5), 1240-1246. https://doi.org/10.1016/j.fertnstert.2003.10.029
xliii Van Heesch, M. M., et al. (2010). Long term costs and effects of reducing the number of twin pregnancies in IVF by single embryo transfer: The TwinSing study. BMC Pediatrics, 10(1). https://doi.org/10.1186/1471-2431-10-75
xliv Sitler, C., et al. (2020). Single embryo transfer versus double embryo transfer: A cost-effectiveness analysis in a Non-IVF insurance mandated system. Military Medicine, 185(9-10), e1700-e1705. https://doi.org/10.1093/milmed/usaa119
xlv Cutting, R. (2018). Single embryo transfer for all. Best Practice & Research Clinical Obstetrics & Gynaecology, 53, 30-37. https://doi.org/10.1016/j.bpobgyn.2018.07.001
xlvi Roque, M., et al. (2018). Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: A systematic review and meta-analysis of reproductive outcomes. Human Reproduction Update, 25(1), 2-14. https://doi.org/10.1093/humupd/dmy033
xlvii Chiware, T. M., et al. (2020). IVF and other ART in low- and middle-income countries: A systematic landscape analysis. Human Reproduction Update, 27(2), 213-228. https://doi.org/10.1093/humupd/dmaa047
xlviii Kamath, M. S., et al. (2020). Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database of Systematic Reviews, 2020(8). https://doi.org/10.1002/14651858.cd003416.pub5
xlix Kamath, M. S., et al. (2020). Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database of Systematic Reviews, 2020(8). https://doi.org/10.1002/14651858.c
l Mersereau, J., et al. (2017). Patient and cycle characteristics predicting high pregnancy rates with single-embryo transfer: An analysis of the society for assisted reproductive technology outcomes between 2004 and 2013. Fertility and Sterility, 108(5), 750-756. https://doi.org/10.1016/j.fertnstert.2017.07.1167
li Gelbaya, T. A., et al. (2010). The likelihood of live birth and multiple birth after single versus double embryo transfer at the cleavage stage: A systematic review and meta-analysis. Fertility and Sterility, 94(3), 936-945. https://doi.org/10.1016/j.fertnstert.2009.04.003
lii McLernon, D. J., et al. (2010). Clinical effectiveness of elective single versus double embryo transfer: Meta-analysis of individual patient data from randomised trials. BMJ, 341(dec21 2), c6945-c6945. https://doi.org/10.1136/bmj.c6945
liii Mancuso, A. C., et al. (2016). Elective single embryo transfer in women less than age 38 years reduces multiple birth rates, but not live birth rates, in United States fertility clinics. Fertility and Sterility, 106(5), 1107-1114. https://doi.org/10.1016/j.fertnstert.2016.06.017
liv McLernon, D. J., et al. (2010). Clinical effectiveness of elective single versus double embryo transfer: Meta-analysis of individual patient data from randomised trials. BMJ, 341(dec21 2), c6945-c6945. https://doi.org/10.1136/bmj.c6945
lv Gelbaya, T. A., et al. (2010). The likelihood of live birth and multiple birth after single versus double embryo transfer at the cleavage stage: A systematic review and meta-analysis. Fertility and Sterility, 94(3), 936-945. https://doi.org/10.1016/j.fertnstert.2009.04.003
lvi Patel, J., et al. (2018). One plus one is better than two: Cumulative reproductive outcomes are better after two elective single blastocyst embryo transfers compared to one double blastocyst embryo transfer. Journal of Human Reproductive Sciences, 11(2), 161. https://doi.org/10.4103/jhrs.jhrs_117_17
lvii Kamath, M. S., et al. (2020). Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database of Systematic Reviews, 2020(8). https://doi.org/10.1002/14651858.cd003416.pub5
lviii Kamath, M. S., et al. (2020). Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database of Systematic Reviews, 2020(8). https://doi.org/10.1002/14651858.cd003416.pub5
lix Peng, Y., et al. (2022). Effectiveness and safety of two consecutive cycles of single embryo transfer compared with one cycle of double embryo transfer: A systematic review and meta-analysis. Frontiers in Endocrinology, 13. https://doi.org/10.3389/fendo.2022.920973
lx Peng, Y., et al. (2022). Effectiveness and safety of two consecutive cycles of single embryo transfer compared with one cycle of double embryo transfer: A systematic review and meta-analysis. Frontiers in Endocrinology, 13. https://doi.org/10.3389/fendo.2022.920973
lxi Mejia, R. B., et al. (2021). Elective transfer of one embryo is associated with a higher cumulative live birth rate and improved perinatal outcomes compared to the transfer of two embryos with in vitro fertilization. F&S Reports, 2(1), 50-57. https://doi.org/10.1016/j.xfre.2020.10.011